The distribution and administration of Covid-19 vaccines are creating unpalatable challenges. On one hand, high-income countries (HICs) are circumventing COVAX, a coalition established to coordinate the equitable distribution of COVID-19 vaccines globally, to enter direct purchase agreements with big pharmaceuticals. The result is the inequitable access to vaccines to low-income countries (LICs) and the continued spread of the mutating virus. On the other hand, anti-vaccination propaganda has caused tremendous vaccine hesitancy and wastage across the world even more so in the HICs where they have stockpiled more vaccines than necessary.
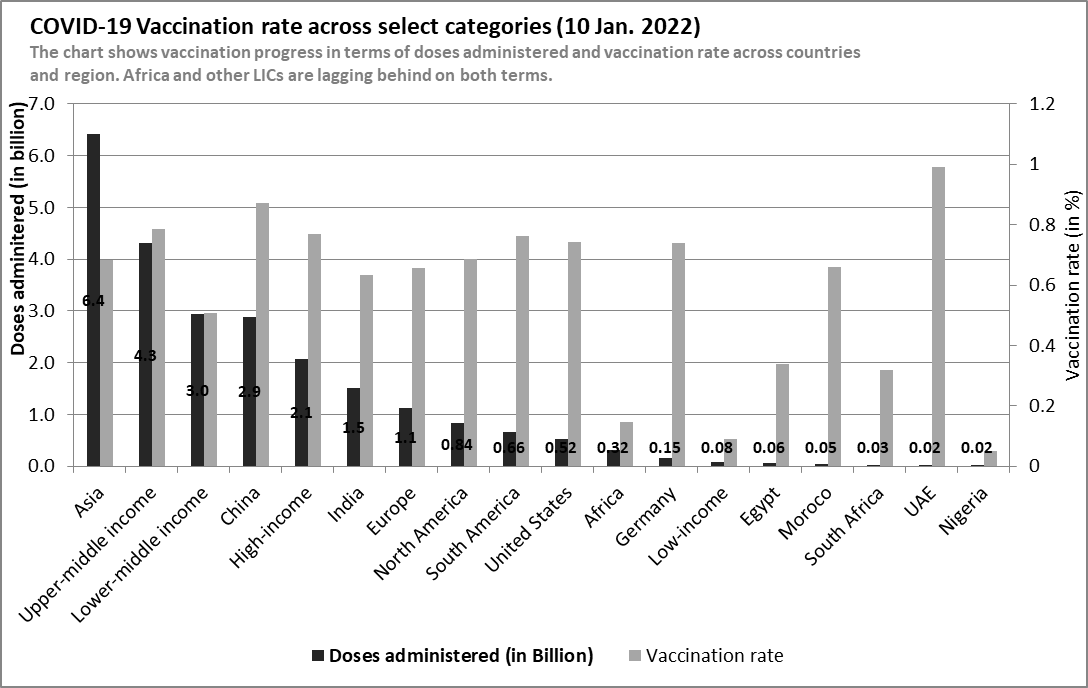
The WHO vaccination data shows that over 17.2 billion vaccine doses have been procured globally. According to data from Our World in Data, about 9.4 billion doses have been administered – representing 54.7% of procured vaccines. As of January 8, 2022, total administered doses represent 59.1% of the global population, of which 49.93% are fully vaccinated and 9.15% are partially vaccinated. HICs and upper-middle-income countries (UMICs) have achieved comparatively high vaccination rates (see figure 1). Figure 1 shows that HICS and UMICs have administered at least 20 times more vaccines than in LICs. Countries such as China, UAE, the US, and Germany have higher vaccination rates than LICs and Africa.

In Africa, the vaccination rate is low compared to other regions – 14.7% (see figure 1). Vaccination in Africa accounts for only 3.3% of vaccines administered globally. The Africa Centre for Disease Control data shows that 58.7% of total vaccines supplied were administered as of 5 January 2022. The total vaccine doses supplied was about 546.7 million doses – roughly 3.1% of global vaccine procurement. As of January 5, 2022, the share of fully vaccinated people was 9.6%; the share of partially vaccinated was 5.1% while booster shots administered was 0.35% of the population. The data shows that Africa lags in terms of total vaccination rate compared to America (72.4%), Asia (68.3%), and Europe (65.7%).
At less than 15% one year after vaccine rollout, LICs show a very slow vaccination rate. This poor vaccination performance is due largely to countries in Sub-Saharan Africa such as Burundi (0.05%), D.R. Congo (0.3%), Chad (1.7%), South Sudan (2.1%), Eritrea (no vaccination), and other countries such as Haiti (1.1%) and Yemen (1.9%). Whilst LICs struggle to meet vaccination targets, high-income countries (HICs) are surpassing their targets, delivering vaccine booster shots against mutating variants of the virus and vaccinating children. Throughout 2021, more booster doses were administered in HICs than the vaccine doses in LICs. This phenomenon has been described as vaccine inequality. Vaccine inequality is due mainly to vaccine nationalism – a situation where national governments exploit bilateral agreements or export restrictions to secure vaccines in advance for their nationals to the detriment of other countries.
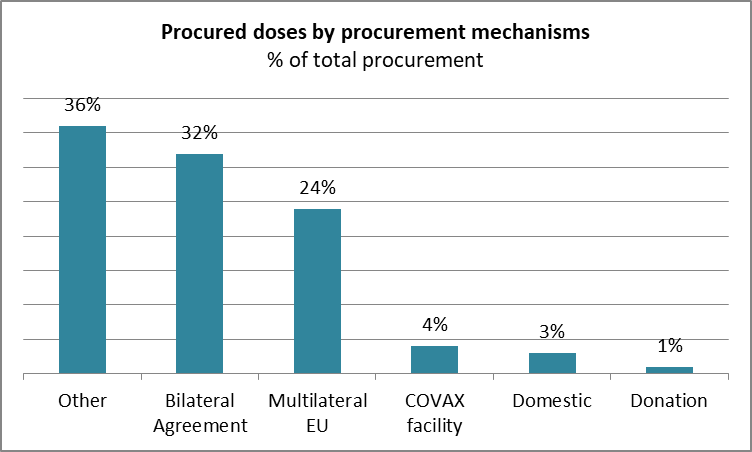
In the early stages of vaccine production, many HICs and middle-income countries (MICs) entered bilateral and multilateral arrangements with pharmaceutical companies to secure surplus quantities of vaccines for their population. The result is an inequitable distribution and access to vaccines and an overall inability to collectively tackle variants of the Coronavirus. The World Health Organization (WHO) warned against such a nationalistic approach to vaccine distribution and formed COVAX in alliance with GAVI, the Vaccine Alliance, and the Coalition for Epidemic Preparedness Innovations (CEPI). COVAX was envisioned to be the primary distributor of COVID-19 vaccines globally to guarantee fair and equitable distribution and access to COVID-19 vaccines for every country in the world. Within COVAX, the Independent Allocation of Vaccines Group (IAVG) serves as an independent referee for a needs-based allocation of vaccines. However, rich nations largely sidestepped COVAX, hoarding doses for their populations and cutting deals directly with LICs and MICs.
The optimistic target for COVAX was to achieve 20% vaccine coverage through COVAX-secured doses by the end of 2021. So far, COVAX has distributed less than 10% of the total vaccine administered globally. According to WHO data, vaccine procurement is largely done under bilateral (32%) and multilateral (24%) agreements. COVAX facilities account for only 4% of purchase agreements (see figure 2). This underlies the vaccine nationalism and inequality arguments, leaving redistribution to vulnerable LICs as an afterthought. COVAX now mainly coordinates and redistributes vaccines to LICs.
Vaccine doses not administered are vaccines wasted
For many HICs, vaccine wastage is partly due to the unwillingness to take the vaccines amongst other issues. In the US, over 15 million doses were wasted since March 2021; France, the UK, and Germany also forecasted high volumes of wastages. By taking a nationalistic approach to vaccine procurement, many countries did not consider the hesitancy that would ensue (see figure 3). Vaccine hesitancy, underlined by the short shelf-life of the vaccines as well as other vaccine administration and policy issues resulted in the observed high vaccine wastages in many countries.
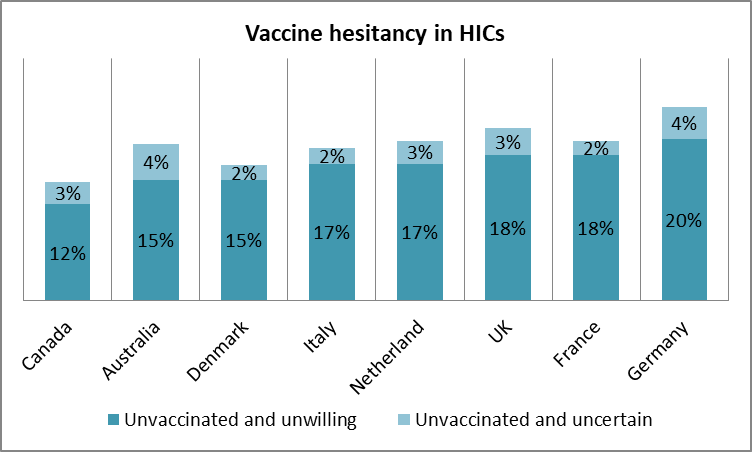
While for HICs, the stockpiling of vaccines for national use and the eventual wastages poses a moral question, for LICs, the story is different. In LICs, vaccine wastage is due to a combination of factors including the short time frame left on donated vaccines, logistical issues and poor infrastructure to deliver vaccination, administrative bottlenecks, vaccine preferences, and hesitancy as well as vaccine racketeering. For instance, in D.R. Congo and Nigeria over 1.7 and 1.1 million doses of vaccines respectively were destroyed due to expiration. Local media reports that the donations were made only a few weeks before the expiry date. As a result, underlined by other logistical and infrastructural bottlenecks, only a fraction of the donated vaccines could be administered. In Kenya, corrupt officials are diverting vaccines for auction at $30 – $50; in other instances, vaccination cards are issued for travel purposes to those not vaccinated.
Nonetheless, juxtaposed with the huge vaccination gaps globally, vaccine wastage is an irony. The excess in the global north is the lack thereof in the global south. A WHO report showed that ninety-eight countries have not vaccinated 40% of their population, and in Sub-Saharan Africa, the vaccination rate is less than 15%. Even though vaccine production has improved (21 approved vaccines) since the rollout in January 2021, vaccines are not distributed fairly and equitably. For instance, less than one in ten health and care workers (HCW) have been fully vaccinated in the African region while four in five have been vaccinated in 22 mostly HICs. Meanwhile, 15 times as many booster doses are currently being administered globally as are primary doses in LICs.
Going forward
COVAX has been working to improve distribution and reduce wastage (to acceptable limits ~5%). To minimize wastage in LICs, COVAX now tries to access the country’s needs for vaccination vis-à-vis their absorptive capacity to distribute and administer vaccines at a level that minimizes wastage. In October 2021, WHO released the Strategy to Achieve Global COVID-19 Vaccination by Mid-2022 with an expanded target to achieve 40% total population coverage by the end of 2021, and 70% total population coverage by mid-2022. Even though the target was not achieved in 2021, with improvement in vaccine production in 2022 and an extensive collaboration amongst HICs, COVAX, pharmaceutical companies, and LICs, it may be possible to surpass the target by the end of 2022.
Currently, governments and firms are resorting to strict vaccine mandate to increase vaccination (for example, Austria, Ecuador, MTN, Citi group). But such strategies can cause massive pushback protests which reverse the gains and increase infections. Therefore, it may be better to be more tactical, use communication and counter-narratives to diminish the spread of anti-vaccine theories. The use of key local stakeholders and trust institutions such as religious houses and family heads may be effective. Vaccine officers must be informed to give vaccination and then register all individuals who present themselves for vaccination. In Nigeria, people have been denied vaccination because they were not pre-registered or scheduled.